Traumatic Injuries
A traumatic brachial plexus injury (TBPI) is a life-altering injury, and may occur along with other injuries. It is important to see a specialist as soon as possible if you suspect you may have a brachial plexus injury. Read more about TBPIs to better understand what you are dealing with and what you should do.
Additional Pages: About Birth Injuries FAQs Terms to Know Find Support
ⓘ TBPI Facts
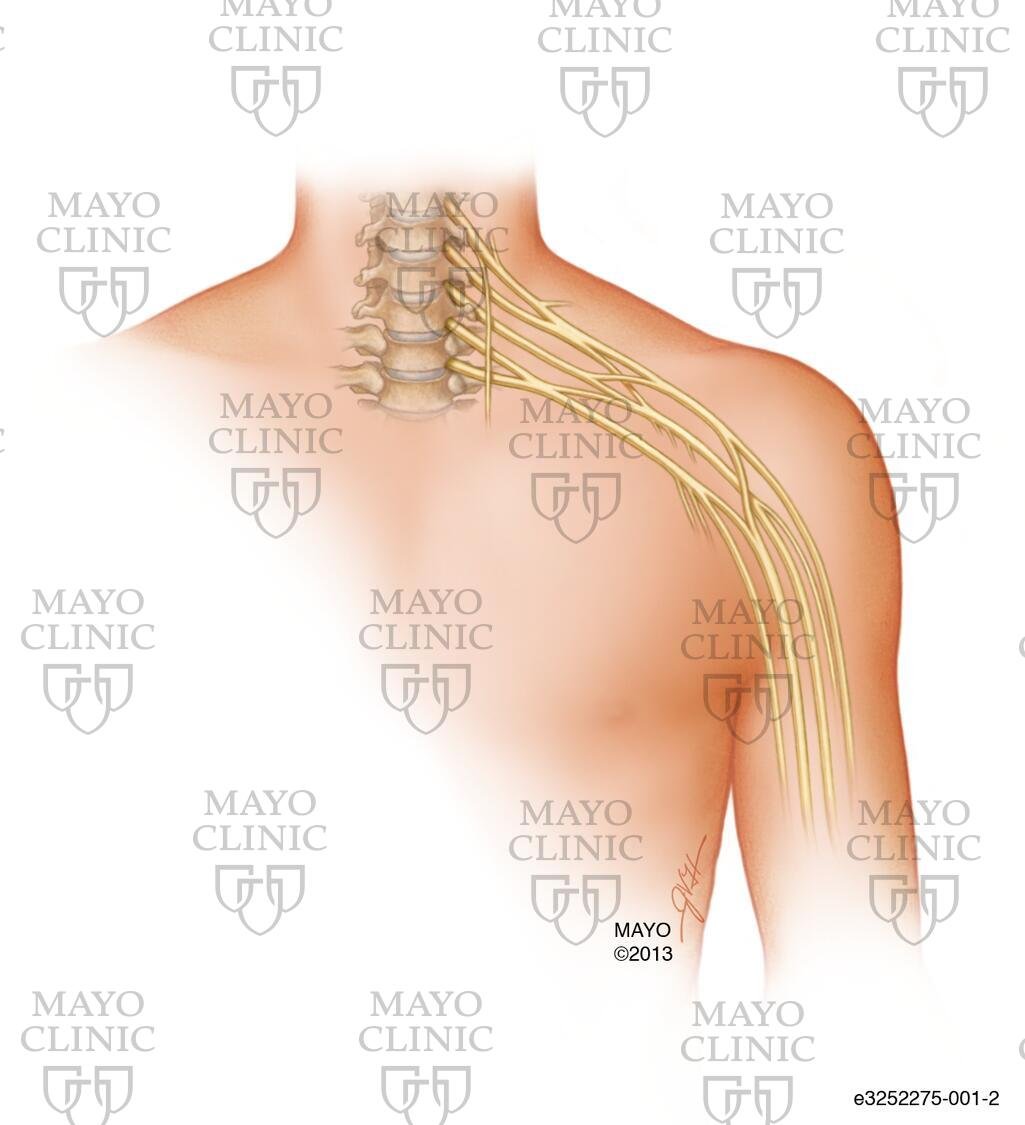
The brachial plexus is the bundle of nerves that exits the spinal cord near the neck and transports signals between the shoulder, arm and hand and the brain. Everyone has two brachial plexuses, one on each side of the neck, though it’s less common to injure both. The nerves exit the spine at the C5, C6, C7, C8, and T1 vertebrae.
A brachial plexus injury is the name for damage to the nerves within the brachial plexus, most commonly due to the nerves being overstretched or torn. While this can happen to anyone, it is unfortunately a fairly common occurrence during the birthing process. An injury caused during birth is known specifically as a brachial plexus birth injury (BPBI).
Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved.
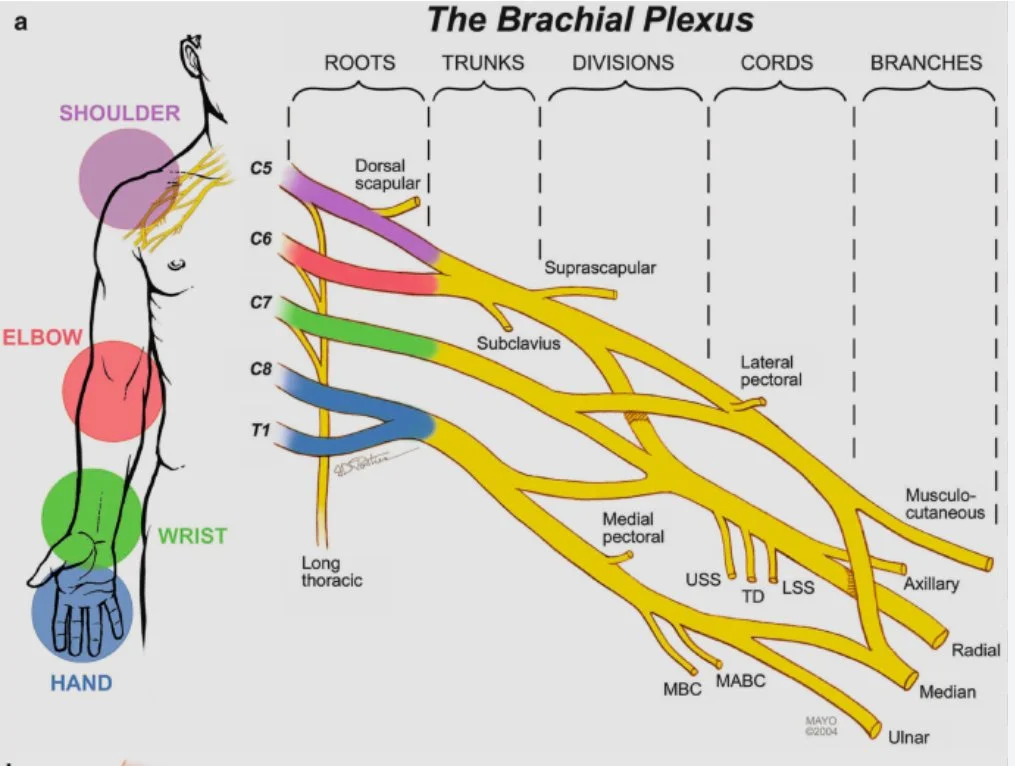
The different areas of the shoulder, arm and hand are controlled and sensed by different nerves within the brachial plexus. As shown below, the C5 nerve generally goes to the shoulder, the C6 nerve the elbow, and so on.
Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved.
-
Brachial plexus injuries can be caused from a variety of things. Physical trauma is the most common, but not the only cause.
Physical trauma causes:
Impact to one’s shoulder in a way that would stretch the neck away from the shoulder, such as motor vehicle accidents or sports injuries
Upward pulling of the arm, such as grabbing a branch while falling from a tree.
Direct trauma caused by a gunshot or stab wound.
Compression or crush injuries can occur if pressure is put on the brachial plexus for a long period of time such as incorrect positioning during surgery or long periods of unconsciousness, or due to anatomical conditions such as thoracic outlet syndrome.
Brachial plexus neuritis can also occur as a result of viral or auto-immune conditions, though these cases are rare. One example is Parsonage-Turner syndrome.
-
Both birth and traumatic brachial plexus injuries can be classified using the same terms. Injuries can range from mild and temporary to complete severing of the nerve(s). In addition, the treatment and prognosis of a BPI depend directly on the extent of injury. Here are different terms used to describe the extent of a brachial plexus injury:
Neuropraxia (stretch) – when the nerves are stretched beyond their elasticity, some individual nerve fibers may be damaged, but the nerve as a whole remains intact. Some mild injuries are temporary and heal completely on their own. In other cases, as the damaged nerve heals a neuroma (scar tissue that has grown around the injury) may form, limiting nerve function.
Neuritis – inflammation of a nerve which can cause temporary or permanent changes in motion and sensation
Rupture – the nerve is torn completely, but not where it attaches to the spine. Surgery must be performed to save the nerve and restore function.
Avulsion – the nerve roots are torn from the spine. Avulsed nerves cannot be repaired as there is currently no way to reattach the nerve roots to the spinal cord.
-
Signs and symptoms of a brachial plexus injury include:
Weakness or not being able to use muscles of the shoulder, arm, and/or hand
Numbness or changes in feeling in the shoulder, arm and/or hand
Intense pain, often described as an electric shock or burning, that shoots down the arm (it is unclear if this pain occurs in infants, but it is very common in people who are injured later in life).
-
Diagnosis
Brachial plexus injuries need referral to a specialist as soon as possible upon detection. Clinical evaluation utilizing a combination of some or all of the following is used to determine the type and extent of injury:
Looking for sensory and motor changes in the affected limb with a physical exam
EMG (electromyogram) and/or Nerve Conduction Studies to determine the presence of nerve signals in the arm
MRI (magnetic resonance imaging) scan to visual the nerves
Possibly CT Myelogram where contrast dye is injected into the spine and scanned to see if there is leakage from the spine or other indicators of damage.
Surgical exploration may be scheduled to physically examine the extent of injury.
Treatment Options
Non-surgical treatments are typically used for more mild injuries or as a supplement to surgery in more severe injuries.
Physical and/or occupation therapy is critical to maintaining range of motion while the nerves are healing, and help retrain muscles after surgical procedures
Medications can help manage symptoms, specifically pain, as needed
Surgical Procedures
Primary (nerve) procedures: Nerve injuries involving complete ruptures or avulsions require surgery in order to see improvement. The type of nerve surgery depends on the extent of the injury. When nerves are repaired, transferred, or grafted, the end of the nerve closer to the hand will not pick up and transfer the signal, but instead acts as a conduit for the upper portion of the nerve to regenerate through. This means that no signal will be able to reach the muscles until the nerve has entirely regrown from the point of injury to the muscle. The regeneration of damaged nerves is slow, about 1 inch or 3 centimeters a month. After nerve surgery, the recovery time frame is months to possibly years, although denervated paralyzed muscle tissue will atrophy and may not be receptive to nerve impulses after a period of time. It should be emphasized that just as the many possible complex variations of the injury occur, so does the rate and extent of recovery for each individual patient. As a general rule the smaller fine control muscles in the hand are in the most danger of being lost. Therefore, by the time any nerve recovery reaches the patient’s hand, atrophy may have resulted in lost function. Some injuries unfortunately do not respond to treatment and are so severe that they are permanent.
Neurectomy/neurotomy – this procedure is used to cut away damaged nerves either for pain relief or in preparation for further surgery
Nerve repair - this may be attempted in the case of more severe stretch injuries or ruptures of a nerve where the two ends of the existing nerve can be reconnected.
Nerve graft - nerves that were torn peripherally (not at the spinal cord) may benefit from nerve graft surgery (typically at 3 to 6 months post trauma) if the two ends of the nerve are no longer close enough to reattach, with the donor nerve being taken from the patient’s leg or other possible site and grafted in place of the damaged section of the brachial plexus nerve(s).
Nerve transfer - A functioning, but less important or extra nerve (such as intercostal nerve) is used to innervate the muscles by making one cut and attaching the portion of the sacrificed nerve that is still connected to the spine to the muscles that need to be innervated.
Musculoskeletal procedures: Besides the nerve grafting and scar tissue removal surgeries available as a possible option, there are other surgical techniques which can be utilized long after the initial period of injury. These include:
Tendon transfer - similar to a nerve transfer, tendon transfers will cut the tendon from when it connects to the bone and move it to another part of the bone so that the muscle can help move the arm in a different direction than it originally did. One example would be moving the tendon for the latissimus dorsi to the shoulder to help with rotation rather than pulling the arm in to the side.
Tendon release - if a contracture occurs, a tendon release may be performed to lengthen the tendon and increase range of motion.
Free muscle transfer - if a muscle has not received signal for too long, it will lose its ability to regain function, even if the nerve is repaired. In this case, a full muscle (usually from the leg) is moved to the arm to perform the function that was lost.
-
“Time is nerve!” Or in other words, time is of the essence. Nerves heal very slowly, and muscles will become unusable if left without nerve signals for too long. If you have been diagnosed with (or suspect) a brachial plexus injury, you should seek a specialist as soon as possible. Find one near you using our directory.
-
Physical Effects
Most people dealing with traumatic brachial plexus injuries (TBPI) have survived life threatening trauma, possibly related to an auto or motorcycle accident or surgical complication. They pulled through and now they are left with a life-altering disability. TBPI have various degrees of severity and no two injuries are exactly the same. Pain is variable for all patients as well. Pain specialists are available; however, everyone has to find their own ways of dealing with the pain. Many find that even “non-medical” ways, such as relaxation techniques and keeping busy can help them escape the pain. Keeping warm and getting plenty of rest can also help. Many people with TBPI deal with chronic pain on a daily basis. Even though nerve pain can be present, so is numbness. Numbness is a big concern because “external pain” can not be felt. Be especially careful when cooking or working with hot items so that you don’t burn yourself. Also, be careful when out in the sun – use plenty of sunscreen on your affected arm, especially if surgical scars are present as that arm may burn faster.
Emotional Wellbeing
Chronic pain as well as life altering injuries can lead to depression. Your emotions will fluctuate up and down. Let family and friends help, but you must also help yourself. The more you do for yourself, the better you will feel. Many of the tasks that you took for granted before your injury will now be a challenge. With practice you will find different ways to accomplish these tasks. An occupational therapist can provide you with many helpful one-handed hints to doing things. Gaining independence is very empowering and will greatly improve your outlook on life. Getting back to school or work will be another great leap towards independence. If at all possible, get back to your place of employment. Not only does this give you independence but it also helps to keep your mind active. Most states have social workers who can assist you with getting an appropriate job. If you were once right-handed, maybe now you have to become left-handed or visa versa. Many schools will allow classes to be recorded or will provide note takers until you can write faster/better. You are not alone! Many people are dealing with brachial plexus injuries. If you have questions or would like to see how other people deal with their injuries visit our (and others’) social media resources.
Asking others for help
There will be times when you need help from others around you. While asking for help is never easy, knowing how to ask can make it easier.
Some situations where you may need help include at the airport, in a restaurant, or ___. You can download our BPI “Assistance Needed” Cards to show the employees to help explain your needs.
Resources & Support
Join the United Brachial Plexus Network in making a difference! Whether you're seeking support, looking for information, or want to connect with others impacted by brachial plexus injuries, we’re here for you. Together, we can raise awareness, provide resources, and advocate for prevention and better care. Explore our network and be part of a global community dedicated to making life brighter for those affected by BPI.